Autism (ASD) and Sleep Guide
This resource will explore the common sleep problems faced by adults and children with autism and review suitable treatment options and strategies for managing sleep-related issues.

Sleep poses significant challenges for many individuals diagnosed with autism spectrum disorder (ASD), affecting both adults and children. Research indicates that up to 80% of young individuals with ASD experience difficulties in falling asleep or maintaining sleep throughout the night. The prevalence of sleep issues is also notably high among adults with ASD, especially those considered ‘low-functioning’. Insufficient sleep can worsen certain behavioural traits associated with ASD, including hyperactivity, aggression, and impaired concentration. Consequently, individuals with ASD who struggle with sleep may face difficulties at work or in educational settings.
This resource will explore the common sleep problems faced by adults and children with ASD and review suitable treatment options and strategies for managing sleep-related issues.
How Does Autism Affect Sleep?
A 2009 study published in Sleep Medicine Reviews observed that parents reported sleep problems in 50% to 80% of children with ASD. In comparison, the rate for children without an ASD diagnosis ranged from 9% to 50%. Additionally, the incidence of sleep issues in children with ASD was higher than in children with other developmental disabilities.
According to the National Autistic Society, the following sleep issues are common among children and adults with ASD:
- having difficulty settling, winding down and going to sleep
- waking repeatedly during the night, or having difficulty getting back to sleep after waking up to go to the toilet
- increased anxiety or an inability to relax causing insomnia
- social cueing problems, where you don’t make the connection between others in the house going to bed and their own need to sleep
- irregular secretion of the sleep hormone melatonin, which regulates sleep patterns, or having atypical circadian rhythms (body clock)
- neurological conditions such as epilepsy
- sensory differences, such as increased sensitivity to blue light from smartphones, laptops and other screens, or sensitivity to certain sounds or white noise, which may be upsetting or distracting and keep you awake
- problems caused by food allergies, which could cause gastrointestinal issues and discomfort, or increased sensitivity to caffeine or other stimulants, which can disturb sleep.
- hypersomnia – sleeping too much. Increased exhaustion could be caused by the additional stress autistic people experience in social situations.
“Sleep problems in ASD, are a prominent feature that have an impact on social interaction, day-to-day life, and academic achievement”
Why Does Autism Affect Sleep?
Individuals with ASD often struggle more with daily pressures and interactions than those without the disorder. Lack of sleep can greatly exacerbate the feelings of distress and anxiety they frequently experience. Consequently, people with ASD who have trouble sleeping may face significant challenges with employment, education, and social interaction, all of which can impact their overall outlook on life.
Studies have also pinpointed several potential causes for these sleep problems that are directly or indirectly related to the individual’s ASD diagnosis. These include:
- Irregular Circadian Rhythm: The circadian rhythm is the 24-hour biological clock that regulates the sleep-wake cycle in humans, influenced by sunlight, temperature, and other environmental factors. This rhythm is processed in the brain and many individuals with ASD show irregularities in their sleep-wake cycle. Furthermore, some studies have noted a connection between children with ASD and irregular production of melatonin, a natural hormone that helps regulate the circadian rhythm.
- Mental Health Disorders: Conditions such as anxiety and depression frequently co-occur with ASD and often result in insomnia and other sleep disorders. Research suggests that up to half of all children with ASD also show symptoms of attention-deficit hyperactivity disorder (ADHD), which can lead to heightened activity and difficulty settling down at bedtime.
- Medical Problems: Epilepsy often co-occurs with ASD, and seizures can significantly disrupt sleep, sometimes regularly in severe cases. Other common medical issues among individuals with ASD include constipation, diarrhoea, and acid reflux, all of which can also affect sleep quality.
- Medication Side Effects: Individuals with ASD who take medication may experience side effects that interfere with sleep. For instance, selective serotonin reuptake inhibitors (SSRIs) can cause agitation and hyperactivity before bedtime. Conversely, antipsychotics such as haloperidol and risperidone may induce excessive daytime drowsiness, leading to difficulties with sleep onset and maintenance.
There is research to suggest there is a possible connection between ASD and obstructive sleep apnea (OSA), a condition characterised by temporary loss of breath during sleep due to airway blockage. Some theories suggest that hypertension found in many infants with ASD may also cause the child’s jaw to develop an irregular shape, potentially leading to sleep-disordered breathing. Other studies have explored links between ASD and disorders like narcolepsy. However, insomnia and parasomnias remain the most common sleep disorders among adults and children with ASD.
Insomnia is the most commonly reported sleep disorder among adults and children with ASD, characterised by difficulty falling and/or remaining asleep on a nightly or semi-nightly basis for more than one month. A study found that 66% of children with ASD reported insomnia symptoms. Similarly, a 2003 study found that 75% to 90% of adults then diagnosed with Asperger syndrome reported insomnia symptoms in questionnaires or sleep diaries.
In addition to insomnia, parasomnias such as frequent nightmares, night terrors, and enuresis (bedwetting) are widely reported among children with ASD, particularly those once diagnosed with Asperger syndrome. The child’s inability to express their fears and discomforts upon waking — often due to ASD — can complicate the way parasomnias are addressed and treated. Moreover, children with ASD often wake up in the middle of the night and engage in ‘time-inappropriate’ activities like playing with toys or reading aloud.
Some effects of a lack of sleep for autistic children can include:
- Increased social communication challenges
- More compulsive rituals and obsessive behaviours
- More frequent occurrences of challenging behaviour
- More instances of hyperactivity and attention deficit disorder
- Higher levels of irritability and aggression
- Higher rates of behavioural issues, depression, and anxiety
- More frequent concentration problems
- More frequent instances of obsessive-compulsive disorder
- Decreased learning and cognitive performance
- Decreased ability to develop peer relationships.
Medication
It’s important to consider that many medications used to relieve autism symptoms may negatively impact the sleep of those who take them. The Autism Research Institute provides a list of drugs and supplements commonly prescribed to treat autism that contains links to documents as well as other information about possible adverse effects.
“Medications should be considered if behavioural interventions are ineffective or difficult to be implemented, especially in individuals with low-functioning autism, and should be used in combination with nonpharmacological strategies, which result in more sustained improvement”
Managing Sleep Problems in Children With ASD
For people without ASD who are struggling to fall asleep or stay asleep, a healthcare provider might discuss the option of medications to help with sleep.
Whilst many of these medications come with side effects and are typically not recommended for long-term use, there can be further complications on top of this for people with ASD.
Often, these medications can carry a high risk of dependency and may exacerbate physical issues associated with ASD, such as acid reflux and constipation. Moreover, sleep-inducing drugs can interact with other medications intended to help individuals with ASD stay focused during the day. Therefore, people with ASD must consult their physician about their current medication regimen before starting any sleep medication.
If someone is considering medication for their child’s sleep, it is important to discuss this with their doctor first as children with autism are especially vulnerable to the risks of dependency and adverse side effects associated with sleep medications and limited evidence exists regarding the use and efficacy of medications for the treatment of sleep disorders in this population group, making prescription drugs a last resort. However, ultimately, as a child’s parent and advocate, their parent/s need to decide what is right for them and their child.
If parents suspect their child with ASD has a sleep disorder, the initial step should be a preliminary assessment. This assessment might include actigraphy, which is a non-invasive objective assessment tool for the study of sleep-wake rhythms, where a child wears a sleep monitor on their wrist to track sleep-wake cycles which monitors neurological and cardiovascular activities during sleep. During this evaluation, parents can assist physicians in ruling out other potential factors affecting their child’s sleep, such as medical issues as well as any medications the child may be taking for ASD. Studies have suggested this is an effective method to evaluate sleep patterns among children with ASD.
Cognitive Brain Therapy (CBT)
CBT is designed to enhance sleep hygiene by educating patients about the science of sleep and helping them develop better nightly habits by focusing on practical methods for altering problematic behaviours and beliefs
“Cognitive behavioral treatment for childhood insomnia (CBT-CI) may improve sleep and functioning in children with autism and their parents”
In the context of improving sleep, CBT can involve maintaining a sleep diary to pinpoint thoughts and behaviours that disrupt sleep. The next step is working to develop more effective attitudes and practices for better sleep. For example learning a relaxation technique like slow, deep breathing. For others, it can help to imagine a calm and relaxing place.
Establishing a Consistent Schedule
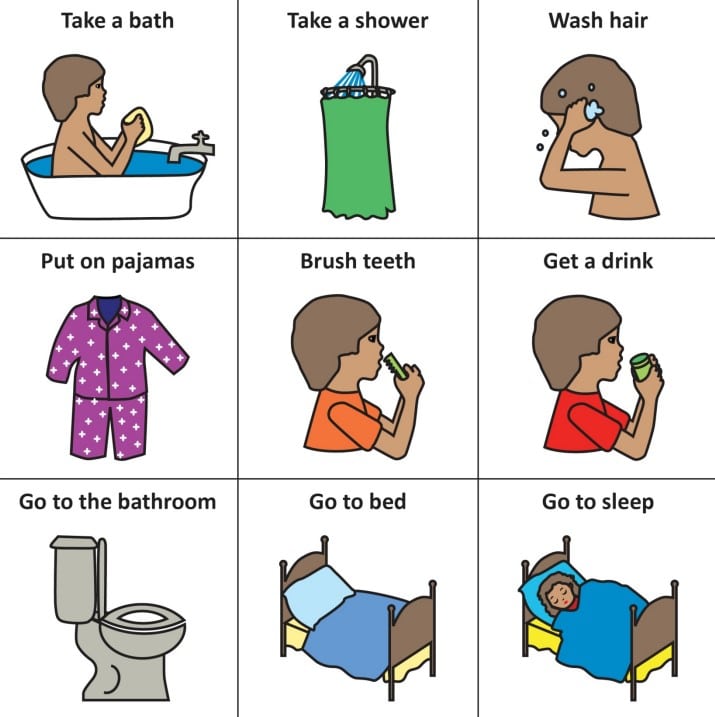
Studies suggest that a bedtime ritual can be crucial for children as it helps establish positive sleep patterns. Create a visual bedtime schedule and choose a reasonable, consistent bedtime. Ensure the entire family adheres to these routines to provide effective reminders. A well-structured bedtime routine will help teach a child to unwind, relax, and prepare for sleep. A sample bedtime checklist could include:
- Putting on pajamas
- Brushing teeth
- Using the toilet
- Washing hands
- Getting in bed
- Reading a book (or being read to)
- Shutting off the light
Additional behavioural interventions may help children with ASD improve their difficulties with sleep. According to a ‘Sleep Tool Kit‘ published by Autism Speaks these interventions include the following:
- Create a visual bedtime schedule that your child will understand. Some children understand checklists; others need pictures, objects, or photographs.
- Limit the number of activities included within the routine. The routine should generally take about 30 minutes or less for your child to complete. Examples are provided below.
- Place stimulating and/or difficult activities early in the evening before the bedtime routine begins. Examples include videos (while enjoyable, they stimulate children), computer/video games, etc.
- Place relaxing and enjoyable activities at the end of the routine, closer to bedtime. Examples include reading a book, listening to quiet music, etc. Keep in mind, that some activities are relaxing for some people and not for others.
- Place the schedule in the area where the routine is performed and at a height that will enable your child to reach each item.
- Choose one cue to let your child know it is time to check his/her schedule and use this cue consistently. Examples of cues include: “time for bed…what’s next?”
Finally, if none of these sleep improvement strategies work, then parents may want to consider prescription medication. In this case, a parent should consult with a physician.
Managing Sleep Problems in Adults With ASD
Nearly 80% of adults with autism experience sleep disturbances. Adults with autism who suffer from insomnia might be advised to undergo acceptance and commitment therapy (ACT). This type of therapy shows promise as an alternative to cognitive behavioural therapy for insomnia, which is typically recommended for adults but may not be suitable or effective for individuals with autism.
Doctors might also prioritise treating any co-occurring medical conditions that could interfere with sleep, such as depression, ADHD, or epilepsy. If these conditions are managed with medications known to have sedating effects, doctors may recommend taking those medications at bedtime.
If none of these sleep improvement strategies work, then patients may want to consider prescription medication specifically designed to tackle problems with sleeping. In this case, a patient should consult with a physician
Therapy and prescription medication can be an effective way to reduce problems associated with sleep disorders and disturbances. However, people with ASD may also experience improvements by establishing a healthy nighttime routine and improving their sleep hygiene.
- Create a calming bedroom environment that promotes sleep. Reserve the bed for sleep only, avoiding activities like eating, watching television, and reading in bed. This helps establish a sleep-friendly atmosphere in the bedroom by confining other activities to different areas of the house.
- Consume balanced dinners and snacks before bedtime, and try to avoid alcohol, nicotine, caffeine, and sugar as much as possible.
- Electronic devices such as TVs, computers, tablets, and smartphones emit blue light, which can hinder melatonin production and delay sleep. Studies suggest avoiding all electronics for at least one hour before bedtime.
- Limit naps to no more than thirty minutes during the day and avoid napping within three hours of bedtime.
- Fluorescent and LED lights emit blue light and other artificial light, which can reduce melatonin production. Outside lights can also affect sleep onset and maintenance. To create optimal bedroom conditions, consider installing dimmable lights to help boost melatonin production, and ensure curtains are drawn to block out external lights and daylight.
- Maintain a comfortable bedroom temperature by adjusting the thermostat according to seasonal changes.
- If you experience nightly discomfort, it might be time to replace your mattress. Most mattresses should be replaced after seven years of consistent use. Your sleep position may also influence comfort; side and back sleepers often find memory foam or latex mattresses more supportive as they conform to the body’s contours and provide spinal support. Innerspring mattresses, on the other hand, may offer less support and contouring for these sleep positions.
- Keep a sleep diary to track nightly patterns and changes. This can be a useful reference for physicians and is often required for cognitive behavioural therapy (CBT)
Additional Resources
- National Autistic Society – Sleep and Autism Guide
- Sleep Foundation – Autism and Sleep Guide
- National Library of Medicine – Autism and Sleep Articles
- Beyond Autism – Autism and Sleep Article
- Living Autism – Autism and Sleep. Ten Possible Strategies